![]()
Definition, Recognition, Documentation, Treatment and Strategic Planning
About SPECC
SPECC | Significant Polyp & Early Colorectal Cancer is a national development programme focussed on the treatment of significant polyps and small (T1) tumours. The programme is being delivered in FREE workshops across England and Wales from 2015 to 2017, helping Colorectal Cancer Multi-Disciplinary Teams (MDTs) deliver consistent treatment options for all patients, wherever they live.
Six core members (inc. surgeon, gastroeneterologist, CNS, radiologist and pathologist) of all colorectal MDTs in England and Wales are being invited to attend a one-day workshop on this complex topic.

Aims of SPECC
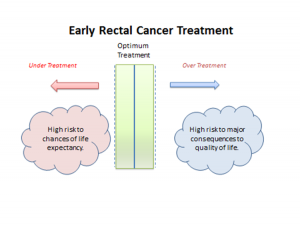
SPECC will help more patients live better for longer, support local cancer services and provide long-term savings for the NHS. It will advance local and regional practice in the definition, recognition, documentation, treatment and strategic planning for significant polyps and early colorectal cancer.
Why and how did we develop the SPECC programme?
Mr Brendan Moran, Consultant Colorectal Surgeon at HHFT Basingstoke, identified the uncertainties and challenges for MDTs discussing SPECC. As the programme developed, these uncertainties became more evident, and we decided that it was a worthwhile topic for a national programme to help colorectal MDTs.
Six graduates from Cranfield University spent a month carrying out a Value Management exercise to identify the key project function for SPECC and provided a full report.
At DDF in 2015, we asked 60 people 4 questions on significant polyp and early colorectal cancer decision-making in their MDT. The replies were:
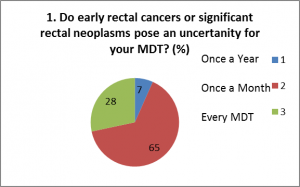
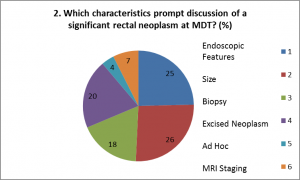
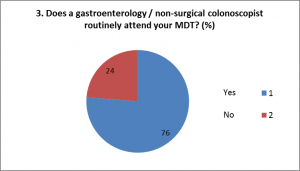
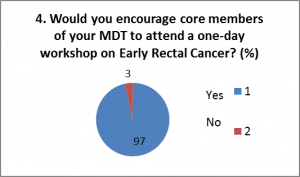
From these we felt that SPECC was a worthwhile programme, of interest to the majority of multi-disciplinary colorectal clinicians and could enhance decision-making for patients with SPECC.
Overview of SPECC Workshop Content
Roll-Out of SPECC
After nearly a year of planning with an eminent steering group, the programme launched in November 2015, and the SPECC faculty have since run the following workshops alongside local faculty:
• London (London Cancer) 06/11/2015
• Bradford (York & Humber) 22/01/2016
• London (London Alliance) 09/03/2016
• Birmingham (West Midlands) 13/05/2016
• Derby (East Midlands) 13/07/2016
• Basingstoke (Wessex) 14/09/2016


Impact of SPECC
We have contacted MDTs through the Pelican contact list and been able to offer 6 free places for each MDT in England and Wales. 383 people from 64 NHS Trusts have joined us at SPECC workshops to date (August 2016).
From the evaluation of the workshops to date, the most common change that people say they will make following their attendance of SPECC is a change at endoscopy:
- ‘Drive to improve our selection/management’
- ‘Look at the detail of polyp characteristics’
- ‘Think twice before attempting polypectomies’
Secondly, many teams, even those with existing specialist MDTs, said that they would put more emphasis on having a specialist SPECC MDT, to allow for even more focussed discussions.
Thirdly, there was greater awareness of the role of biopsy for SPECC and the potential risks to future treatment options.
Online Resources for Delegates
“A word about the extremely important SPECC programme, which I attended recently in Basingstoke. Brendan Moran and his team’s enthusiasm, knowledge and commitment to this programme are extraordinary.”
ACPGBI President 2016-17, Mr Peter Dawson
SPECC Basingstoke 14.9.16
“Excellent day: thought-provoking topics & discussions.”
Delegate at SPECC East Midlands 13.7.16
“Case studies were most useful.”
“Very interesting, well organised, fascinating.”
Delegates at SPECC West Midlands 13.5.16
“Very influential meeting.”
“Excellent workshop with expert speakers.”
Delegates at SPECC York & Humber 22.1.16
Funding for the SPECC programme has been the greatest challenge to date. We received generous support from Applied Medical (1st workshop), Exact Sciences (first 4 workshops) and Norgine (first 10 workshops).
We were also fortunate to receive some grants from charitable trusts towards the costs of SPECC.
Otherwise funding has come from charitable donations to Pelican and the charity’s reserves.
If you would like to support this important programme, please contact Pelican
Read more about Partners and Sponsors
SPECC Leads, Steering Group and Faculty
Clinical Lead:
Mr Brendan Moran (Consultant Colorectal Surgeon, HHFT Basingstoke)

Other leaders in the field, from hospitals around England and Wales, are helping to develop and deliver the programme:
Local Leads:
Mr Ayan Banerjea (Surgeon, Nottingham)
Mr John Grabham (Surgeon, Surrey and Sussex Healthcare NHS Trust)
Mr Jim Hill (Surgeon, Manchester)
Mr Stephan Korsgen (Surgeon, Heart of England)
Mr Jonathan Robinson (Surgeon, Bradford)
Prof Matt Rutter (Gastroenterologist, University Hospital of North Tees)
Mr Jared Torkington (Surgeon, University Hospital of Wales)
Mr Paul Ziprin (Surgeon, London)
The Steering Group and Faculty:
Dr Richard Adams (Oncologist, Cardiff)
Professor Wendy Atkin (Epidemiologist, Imperial)
Dr Svetlana Balyasnikova (Radiologist, Royal Marsden)
Dr Conrad Beckett (Gastroenterologist, Bradford)
Prof Pradeep Bhandari (Gastroenterologist, Portsmouth Hospital)
Mr Neil Borley (Surgeon, Cheltenham)
Dr Corinne Brooks (Gastroenterologist, HHFT Basingstoke)
Professor Gina Brown (Radiologist, Royal Marsden)
Mr Wayne Croves (Clinical Nurse Specialist, Nottingham)
Mr Chris Cunningham (Surgeon, Oxford)
Mr Mit Dattani (Pelican Research Fellow)
Dr Amandeep Dhadda (Oncologist, Hull & East Yorkshire)
Dr Sunil Dolwani (Gastroenterologist, Cardiff)
Mrs Sarah Duff (University of South Manchester)
Dr James East (Gastroenterologist, Oxford)
Dr Colm Ford (Radiologist, QE Birmingham)
Dr Ian Geh (Oncologist, Birmingham)
Dr Rob Glynne-Jones (Oncologist, Mount Vernon)
Dr Mark Goldstein (Radiologist, Heart of England)
Ms Donna Kellett (Advanced Nurse Practitioner, Bradford)
Dr Gerald Langman (Histopathologist, Birmingham)
Dr Andy Lowe (Radiologist, Bradford)
Mr Michael Machesney (Surgeon, London)
Dr Brian McKaig (Gastroenterologist, Wolverhampton)
Dr Jamie Mills (Oncologist, Nottingham)
Mr Michael Hershman (Surgeon, Wolverhampton)
Mr Mark Peacock (Surgeon, Gloucestershire)
Dr Andrew Plumb (Radiologist, UCL Hospitals)
Mr Rupert Pullan (Surgeon, Torbay)
Professor Phil Quirke (Pathologist, Leeds)
Prof Krish Ragunath (Gastroenterologist, Nottingham)
Mrs Nicky Richards (Clinical Nurse Specialist, HHFT)
Dr Velauthan Rudralingam (University of South Macnhester)
Professor Brian Saunders (Gastroenterologist, St Marks)
Professor John Scholefield (Professor of Surgery, Nottingham)
Mr Adam Scott (Surgeon, Leicester)
Mr William Speake (Surgeon, Royal Derby)
Mr John Stebbing (Surgeon, Royal Surrey)
Professor Bob Steele (Surgeon, Dundee)
Mr Mark Steward (Surgeon, Bradford)
Dr Alex Stewart (Oncologist, Royal Surrey Hospital)
Prof Arthur Sun-Myint (Professor of Clinical Oncology, Clatterbridge)
Dr Claire Taylor (Nurse Consultant, St Mark’s)
Prof Jan van der Meulen (Epidemiologist, LSHTM, London)
Dr Nick West (Histopathologist, Leeds)
Mr Graham Williams (Surgeon, Wolverhampton)

