MRI (Magnetic Resonance Imaging) images can be carefully analysed to provide accurate information about colorectal cancer tumours before surgery – and after. For example, MRI can provide information on the exact site of the tumour, the depth of tumour invasion and whether lymph nodes are involved. This helps greatly in planning effective surgery. The radiologist can also indicate whether there is an opportunity to potentially shrink high risk tumours prior to surgery (using pre-operative radiotherapy, for example) or to avoid needless preoperative therapy in patients with good prognosis tumours.
Here, we go into further detail about what MRI reveals, and why imaging plays such a vital role in improving patient outcomes:
Imaging underpins all aspects of managing this disease through the patient`s journey and we hope that the advances in diagnosis, imaging-directed preoperative treatment, surgery and surveillance will continue to improve outcomes for patients with colorectal cancer.
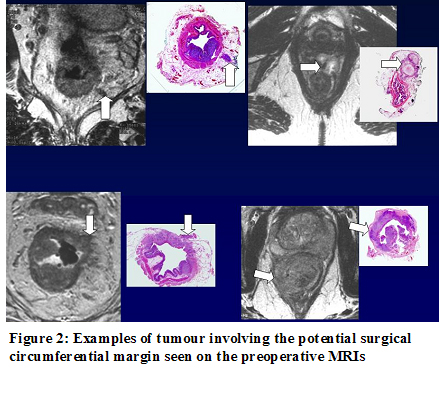
High resolution MR images show a high degree of resemblance to tumour pathology sections that are obtained after surgery (figure 1).

By careful comparison of these images with histopathology sections, we have learnt to read MR images to give us accurate information about the depth of tumour invasion and whether lymph nodes are involved. In addition, further important information can be obtained such as the precise distance of tumour from the planned surgical excision (the potential circumferential resection margin, figure 2) whether or not the tumour has invaded into blood vessels (figure 3), the peritoneum (figure 4) and the height from the anal sphincter (figure 5).
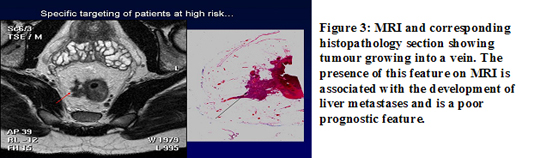
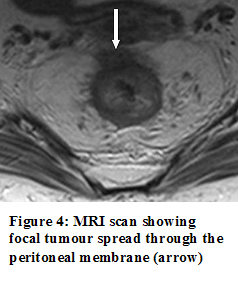
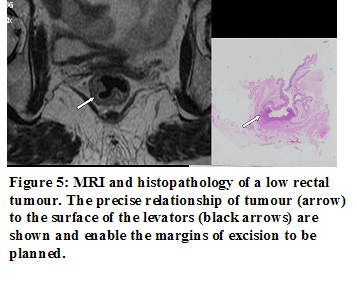
All of this information enables precise treatment planning and provides a method of tailoring preoperative treatment to the patient`s individualised risks of local and/or distant relapse.
Until recently these variables would only have been detected on the final surgical specimen thus missing the opportunity to potentially shrink high risk tumours prior to surgery and to avoid needless preoperative therapy in patients with good prognosis tumours.
Increasingly, clinical trials are incorporating MR assessment of prognostic factors prior to therapy to enable objective comparison of treatment modalities and outcomes that are targeted to preoperative prognostic subgroups. By comparing pre-treatment MR staging with post therapy histology assessment a quantifiable assessment of the efficacy of particular treatment protocols can be achieved.
Professor Gina Brown is the NHS lead in imaging research at the Royal Marsden Hospital. She also holds honorary positions with the Institute of Cancer Research and Imperial College London, and has long-established research links with the Pelican Cancer Foundation in Basingstoke, who are a charity committed to developing and teaching improvements in cancer surgery and providing research funding for various projects throughout the UK and Europe.
The Royal Marsden’s imaging department has a strong track record in multi-disciplinary research that has led to improvements in staging and tumour assessment in the common cancers and thereby changed clinical practice. The imaging portfolio underpins much of the clinical trial research that is undertaken within the hospital, and novel imaging techniques have been established as a result of this and have had a significant impact on patient care with rapid dissemination into the wider clinical community through established training and development programmes and publications.
Professor Brown has responsibility as the RMH imaging research lead for coordinating the integration of innovative imaging techniques into clinical trials supported by NHS Technology Platform Funding, thus strengthening our international reputation in cancer research.
NIHR support enables the cancer imaging team to conduct research leading to an increase in the use of state of the art imaging in all aspects of the patient journey, from diagnosis to management of recurrent disease.
A successful example of the roll out of such research resulting in changes in UK medical practice, has been the mentoring of 186 multi-disciplinary teams and development of imaging in colorectal cancer, through the National MDT-TME training programme, hosted by the Pelican Cancer Foundation.
As cancer imaging representative on the NCRI Colorectal Clinical Studies Group and Subgroups, her role has been to ensure that high quality imaging is embedded into national clinical trials protocols as a means of introducing best practice to routine clinical care, e.g. innovative trials such as Aristotle, FOXTROT Study, and the multi-centre RMH-led EXPERT-C trial, all incorporating high-quality imaging.
In collaboration with colleagues at St George’s Hospital, she contributes to a training programme for academic clinical research fellows in radiology and Clinical research lecturers in cancer imaging, developing an active programme which enables radiologists to pursue an academic career in cancer imaging.
Professor Brown has provided educational material for many national and international courses,and authored chapters in two major educational text books in 2007, as well as edited and co-authored Contemporary Issues in Cancer Imaging: Colorectal Cancer.
